
This was my view while I gave blood...a pissed off ZJ who wasn't allowed to be with me.

The day before surgery we had to be at the hospital from 8:00 am to 12:00 pm. ZJ had an EKG, chest xray, her urine collected and blood drawn. We also met with people from several hospital departments.
The evening before surgery we kept ZJ up very late and gave her a big snack since she wouldn't be able to breastfeed after 3:00 am or have any breakfast that morning. She was cranky the next morning but exhausted. She slept on me and in the car on the ride to the hospital.
We had to be at the hospital at 6:00 am. In the pre op area ZJ donned her gown and just before they were ready to take her back she got a dose of Versed, which tastes horribly and pissed her off. A few minutes later she became loopy and adorable, which was a pleasant way to see her go. They carried her off to surgery at 8:05 am.

We were then sent to the CVICU/Surgery waiting room and given a pager. This area had recliners for family to sleep in since no one is allowed to sleep in the ICU, bathrooms, showers, a kitchen, seating areas and private pumping rooms (which I used because I wasn't allowed to breastfeed until ZJ was out of ICU). We were told we would get paged every 90 minutes or so for updates. We would then go into a private room and wait for the surgeon's nurse practitioner to come and update us.
These were the updates we were given:
9:15 am: ZJ was asleep, all her lines were in, she was doing well, the echo was done
11:00 am: the surgeon had opened her sternum, her heart was stopped and she was on the bypass machine, she was doing well, the surgeon was assessing her malformations
12:30 pm: the repair was complete, her heart was restarted and the bypass was stopped, the post op echo was done, the surgeon was going to close her incision
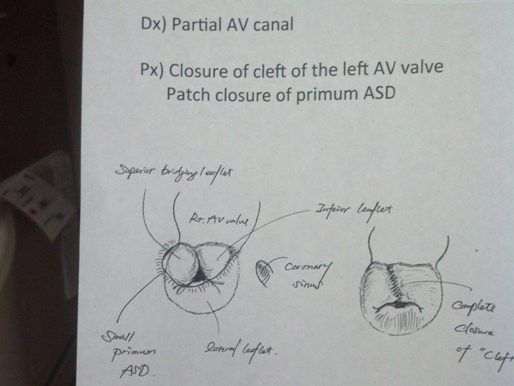
At 1:00 pm the surgeon came to discuss how everything went. He explained how the mitral valve was repaired with stitches and her ASD was patched with her pericardium. He was pleased with the outcome and would not expect her to need more surgery in the near future.
We were not able to go see her until 3:15 pm when we were finally sent to CVICU. She was already extubated, on an antihypertensive, an inotrope and light sedation. She was getting her own blood back from the cell saver and whole blood the bypass machine had been primed with (not my blood, since I only gave platelets). She was on oxygen, and morphine as needed. She had a chest tube to drain fluid, central line in her neck for drugs and fluid, IV in her foot, arterial line in her wrist for continuous blood pressure monitoring, and a catheter to measure urine output. Both of her arms were restrained.

From the time we got there she would regularly wake, grimace, silently cry and hold her breath. The silent crying was likely due to having been intubated. It took several hours for her voice to return. Her nurse was surprised by how long she would hold her breath every time she woke angry and would try to get her to breathe each time. We would try to comfort her by talking to her and rubbing her head, but would just have to wait for her to fall back asleep for her to be peaceful.
During the evening her supplemented oxygen was reduced so her mask was removed and a nasal canula was used instead. She only needed a little of the blood and never received any of mine. At this point we didn't understand why only platelets were taken from me when she only received whole blood and her own blood.
Most of the ICU had private rooms but at the very end there was space for 6 babies. It was the under 1 year section. The private rooms were full so we had to be in this more public area. We had no plans of leaving her alone at any point and even though everyone told us we weren't allowed to sleep in the ICU, our surgeon had told us we could. Upon clarification we were told if we fell asleep in a chair we wouldn't be asked to leave, it's just that we couldn't take up any extra room. Once I saw the area and chairs, I knew I couldn't sleep there so we took the offer for a Ronald McDonald room which we were told were reserved for families the night of surgery. We split the night so I had the room from about 9:00 pm to 2:00 am and NJ had it from the time I got back to the ICU till 7:00 am. I did very little sleeping in my first "night" ever away from ZJ but at least I got a little and a shower too.
This is a diagram of her repair which was taped to the end of her bed.
During the night both drugs were stopped. She had longer periods of alertness on Thursday and more content/quiet moments, not just crying every time she woke. But she still wouldn't really look at me, she seemed to look through me, and still slept a lot. She had been on clear liquids after surgery and couldn't handle her straw cup so had her first ever baby bottles and nipples to suck down the tiny amounts of water she was allowed (about 1 oz per hour) and a few hours later, to drink the breastmilk I had pumped. I was surprised that even while sedated and out of it, she would say "wawa" when she wanted to drink. On Thursday she was allowed food and ate almost all of an applesauce cup I had brought from home. She refused all other food the rest of the day and frequently refused fluids too.

By midday they were running out of room in the ICU and were going to squeeze us in between two other babies. Then suddenly the plan switched to sending us to the 16th floor, CV acute care, that afternoon. I was very excited about this because on the 16th floor each room has a pull out bed for family and a private bathroom and shower. In order to move she needed several of her lines pulled out. They took out her catheter, removed the oxygen, took out the arterial line, moved her IV from her foot to her arm because it was no longer working and took the central line out. They also disconnected her chest tube from a box that applied suction and measured the output and connected it to a little plastic bulb they called a "grenade" that was portable and would be dumped and measured every few hours. While we waited to move we got to hold her for the first time, since she had to be switched from a full size bed to a crib for transport.
Around 3:00 pm, 24 hours after we got to see her in ICU, she was wheeled to the 16th floor. Our ICU nurse advised me to take her out of the crib and put her in the full size bed already in the room so that I could sleep with her/breastfeed her. As soon as we got in the room I laid her on the bed and let her breastfeed. After that she seemed to finally acknowledge me and look at me. I think she was mad at me before and was refusing to look at me. We let the nurse know that I would be cobedding with ZJ and we had to sign a waiver to do so since she is under 2 years old. The rest of our stay ZJ and I slept in the hospital bed and NJ slept on the couch/bed.

The nurse removed her sternal dressing and cleaned the tape over her incision with betadine. We then had to clean it with betadine twice a day until our post op appointment. She also helped us get some of the adhesive off her body, clean her up a bit and dress her.

We didn't realize that they no longer had her on a schedule to receive pain medications and during the evening she began to show signs of pain. She was grunting and scratching her neck and chest. We told the nurse she needed something and found out they don't have her medication, Hycet, on the unit and would have to order it. It ended up taking 2 hours and 15 minutes to get her pain drugs. The medication never came. NJ had to find the resident who looked up ZJ's info and saw that she could have morphine, which was on the unit, so we had them give her that. This was after she was in so much pain she fussed and passed out TWICE. We were not happy and were wishing we were still getting the immediate care received in the ICU. We also had them set up a schedule for the medication so it would be here when needed and this would not happen again. After that she received Hycet every 6 hours at 3:00 and 9:00. We were also concerned that she was refusing all food and drink so over night they set up an IV to give her fluids.

When ZJ woke up Friday she seemed more alert but was still quite grumpy. Here she is scowling at the pretty flowers Auntie S brought her the evening before.

Every 4 hours her blood pressure, temperature and oxygenation was measured by the patient care assistant. Every day in the hospital she had a chest xray in her room. Every 6 hours she had her pain meds which she hated the taste of. In between all of that there were physical therapists, cardiologists, residents and nurses coming in to her room. She hated and was terrified of all of them, except the PCAs. She learned quickly that nothing the PCAs did hurt her so she would sit and cooperate with them and even speak to them. But for everyone else she would cling to me. The first few days she couldn't move so her eyes would get big when her door opened and she would just wait, terrified to see who was coming. After she was back to moving about she would get on me and smash herself into me. She would yell "Mama" when anyone would come near.
When the cardiologists came by Friday morning they mentioned getting her up and out of bed. I told them I thought I should wait until she was eating a bit but they said as long as she was drinking, which she was doing a little of at that point, that she was fine to move around and that it was good for her recovery. So we got her dressed and let her walk for the first time. She walked all the way to the other side of the unit where we checked out the toy room, picked up some toys to bring back to her room and she tried out every vehicle available and drove around a bit. This seemed to brighten her spirits and from then on she seemed more like herself.
On Saturday she was looking and acting much more like herself. I was surprised at how quickly she got back to her usual nap and night schedule. We did more walking and driving and switched out her toys. For the most part the pain meds every 6 hours were covering her needs but we had a few incidents here and there when she displayed signs of pain and one time was pretty upset and scratched the skin off of her neck. The surgical fellows, who also visited each day, took her chest tube out on Saturday. She did not like this. They gave her morphine, removed the tube and tightened the stitch.
We were told to expect a Monday discharge, knowing we needed an EKG and echo before we could go home and we probably couldn't do the echo on a Sunday. But, her surgeon came by Saturday and thought she looked great. He didn't want her sitting around all weekend if she didn't need to be here because of the risk of her getting sick. He said he'd talk to the cardiologists and that he recommended we go home on Sunday.

On Sunday she was doing so well we decided to hold off on the 9:00 am pain meds and start delaying them a few hours to see what she needed at that point. She was very active and I was getting very antsy to get home where we could adequately entertain her. She ate very little the entire hospital stay and might not eat something one day that she'd eaten the day before but she was drinking consistently.


The cardiologists came by and said she would have an EKG and be discharged if it was normal. We would just wait to do the echo till her post op visit the following Friday. She freaked out when the person came to hook her up to the EKG machine but her nurse brought some little toys for her and she calmed down and forgot about the test. We went home Sunday afternoon. We have to be careful for 6 weeks while her breastbone heals. We can't pick her up from under the arms and we need to try to keep her from climbing, pulling and falling. We also will try to keep her healthy because even a regular cold could affect her lungs which are impacted from being on the bypass machine.
At home ZJ was extra clingy to me, which was to be expected, but other than that acting pretty normal. We gave her pain meds each night and only occasionally during the day. The last pain meds she had was during the night prior to her post op visit.

On Friday we went to her post op appointment.

At this appointment she had an EKG, chest xray, echo and the tape and stitches removed. They wanted to do a sedated echo but I told them prior to the appointment that I wouldn't be putting her through that. I brought some brand new toys to try to entertain her through the echo but she was too freaked out to stay calm. We got through it though and I'm glad we didn't sedate her.
Here she is just after the stitch removal.

This is from the following Monday, July 1.

No comments:
Post a Comment